This year the world should have been “talking about the virtual elimination of HIV” in the near future. “Within five years,” says Prof Sharon Lewin, a leading researcher in the field. “Now that’s all very uncertain.”
Scientific advances had allowed doctors and campaigners to feel optimistic that the end of HIV as a public health threat was just around the corner.
Then came the Trump administration’s abrupt cuts to US aid funding. Now the picture is one of a return to the drugs rationing of decades ago, and of rising infections and deaths.
But experts are also talking about building a new approach that would make health services, particularly those in sub-Saharan Africa, less vulnerable to the whims of a foreign power.
The US has cancelled 83% of its foreign aid contracts and dismantled USAid, the agency responsible for coordinating most of them.
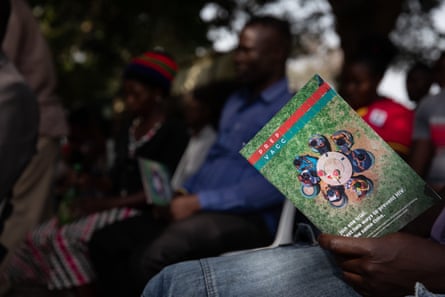
Many fell under the President’s Emergency Plan for Aids Relief (Pepfar) programme, which has been the backbone of global efforts to tackle HIV and Aids, investing more than $110bn (£85bn) since it was founded in 2003 and credited with saving 26 million lives and preventing millions more new infections. In some African countries it covered almost all HIV spending.

There is a risk, says Lewin, director of the Doherty Institute, a joint venture of the University of Melbourne and Royal Melbourne Hospital, and past president of the International Aids Society, of “dramatic increases in infections, dramatic increases in death and a real loss of decades of advances”.
There is no official public list of which contracts have been cancelled, and which remain. It appears that virtually no HIV-prevention programmes funded by the US are still in operation, save a handful principally providing drugs to stop pregnant women passing on the infection to their babies. Countries report disruption to the most basic measures, such as condom distribution.
TimelineEight key dates in the fight against Aids and HIV
Show
The first reports of a mysterious, deadly illness affecting gay men in the US appear in scientific journals.
Scientists at the Pasteur Institute in Paris report the discovery of a virus that could be the cause of Aids – now known as HIV.
The first antiretroviral (ARV) drug to fight HIV and Aids is approved by the US Food and Drug Administration. The 1990s will see huge advances in treatment that see deaths plummet for those who can afford the drugs.
Generic pharmaceutical companies offer to produce cheaper forms of ARVs for developing countries. There are over 20 million people living with HIV in Africa but virtually no access to the drugs.
The President’s Emergency Plan for Aids Relief (Pepfar) is announced by George W Bush to address HIV and Aids in hard-hit countries worldwide. It will eventually invest over $110bn (£84bn) and prevent millions of infections and deaths.
The first cure: doctors announce that Timothy Ray Brown of San Francisco is free of HIV after undergoing a bone marrow transplant to treat leukaemia.
The UN sets a Sustainable Development Goal (SDG) to end Aids as a public health threat by 2030.
Sweeping cuts to US aid funding leave HIV patients worldwide facing a dangerously uncertain future.
Some treatment programmes have been spared, but not those whose focus conflicted with the Trump administration’s war on “gender ideology” or diversity, equity and inclusion (DEI), such as those working with transgender communities. Doctors, nurses and other healthcare workers have been laid off, while worried patients are hoarding drugs or stretching supplies, according to UNAids surveillance. UNAids itself has lost more than half of its funding.
Even programmes that have survived the cull have faced turmoil since February, with instructions to stop work rescinded but with no certainty that funding will continue.

In only one example, the Elizabeth Glaser Paediatric Aids Foundation says it has had to halt HIV treatment for 85,000 people in Eswatini, including more than 2,000 children, and tests for thousands of pregnant women and babies to prevent transmission and begin life-saving medication.
Access to drugs represents an “immediate crisis”, Lewin says. “If people with HIV stop the medications, then not only do they get sick themselves, which is tragic, but they also then become infectious to others.”
As clinics on the frontline of treating the disease scrabble to secure access to basic drugs, scientists at this month’s Conference on Retroviruses and Opportunistic Infections in San Francisco were hearing that HIV might soon be preventable with a once-a-year injection.
Quick GuideHIV and Aids around the world: in numbers
Show
630,000
The number of people who died from Aids-related illnesses in 2023 – more than one every minute. Since the epidemic began, a total of 42.3 million people have died.
1.3 million
The number of new infections in 2023, mainly in sub-Saharan Africa. Women and girls accounted for 44% of these.
39.9 million
The number of people around the world living with HIV. Of these, 30.7 million are accessing antiretroviral therapy.
51%
The percentage by which the death rate has fallen in just over a decade. The risk of an HIV-positive mother passing the virus on to her baby is now less than 1%.
$19.8bn
The amount of funding available for Aids response in low and middle-income countries by the end of 2023. Of this, 59% came from domestic sources. International funding dropped by 7.9% between 2020 and 2023.
The drug lenacapavir was already generating huge excitement in the field, after trial results showed that a six-monthly jab could prevent HIV. New results from the manufacturer Gilead suggest that a tweak to the formula and how it is given could see its protective effects last even longer.
Nevertheless, Lewin says, the mood at the meeting, packed with many of the world’s leading HIV specialists, was “dire”.
As well as programme cancellations, there are “huge concerns around science and what’s going to happen to the [US] National Institutes of Health, [whose] funding of science has been so significant on every level”, she says.
Some scientists in receipt of US funding have been told to remove their names from DEI-linked research, she says, even though DEI is fundamental to the HIV response.

“I don’t mean that in a sort of touchy-feely way, I mean that’s what we need to do: you need to actually get those treatments to these diverse communities.”
In 2022, 55% of all new HIV infections were within “key populations”, such as gay men, other men who have sex with men, sex workers, transgender people, prisoners and people who inject drugs.
Prof Linda-Gail Bekker, of South Africa’s Desmond Tutu Health Foundation, has seen US funding for three trials of potential HIV vaccines involving eight countries cancelled and only reinstated after an appeal to the US supreme court.
“We’re running around like chickens without heads to at least get one going, because the vaccines are sitting in the fridge and will expire,” she says.
She led the lenacapavir trial that showed it offered 100% protection to young women in sub-Saharan Africa, but now worries about HIV/Aids prevention “falling off the radar completely”.
The global community had been making headway towards the United Nations’ goal of ending Aids by 2030, she says, with a five-year plan to use “amazing new innovative tools and scale them up”, which would have led to “less dependence on foreign aid and more self-reliance” as new infections fell and attention shifted to maintaining treatment for people with HIV.
“All of that is hugely at risk now because, without these funds, our governments will have to step up but they will concentrate on treatment,” she says. “We know they will do that, because that is what we did for the first 30 years.”
Efforts to control Aids were entering “the last mile”, which was always likely to be more expensive, she says. “The people who were happy to come into health facilities, they would have come into health facilities.”
It would be difficult to rely on government funding to reach the remaining groups, she says, not only because of fewer resources but also because in some countries it means targeting groups whose existence is illegal and unrecognised, such as sex workers or sexual minorities, and young girls may be reluctant to use government clinics if they are not supposed to be sexually active.
“I feel like the odds are very stacked against us,” says Bekker, adding: “We’re obviously going to have to re-programme ourselves [and] formulate a different plan.”
Pepfar had pledged funding to the Global Fund to Fight Aids, Tuberculosis and Malaria, to deploy 10m doses of lenacapavir in low-income countries. While the Global Fund has promised to maintain its commitment, it might receive fewer than the planned number of doses, Bekker fears.
“Six months ago, I was saying the best thing we can do with lenacapavir is offer it to everybody in a choice environment. [Now] I think we’re gonna have to say who needs [injectable] prep,” she says, “and the rest have to do the best they can.
“How do we make that decision? And what does that look like? It is back to sort of rationing.
“When we started ARVs [antiretroviral drugs] way back in 2000,” Bekker recalls, “you would go, ‘you get treatment; you don’t, you don’t, you don’t’.
“It feels terrible … but you have to get over that. You have to say it will be infection-saving for some people. And we’ve got to make it count.”
For Beatriz Grinsztejn, president of the International Aids Society, the disruption is critical and threatens many vulnerable people. But, she adds, it could present “an important opportunity for ownership – otherwise we are always left in the hands of others”.
She worries about the impact of cuts to funding on younger scientists, with their potential loss from the research field “a major threat for the next generation”. But, she adds, the HIV community is “powerful and very resilient”.
There have already been calls for new ways of doing things. It is “time for African leadership”, members of the African-led HIV Control Working Group write in the Lancet Global Health. There are now plans for Nigeria to produce HIV drugs and tests domestically.
Christine Stegling, deputy director of UNAids, says it began “a concerted effort” last year to develop plans with countries about how their HIV programmes could become more sustainable domestically “but with a longer timeframe … now we are trying to do some kind of fast-tracking”.
Governments are determined, she says, but it will require fiscal changes either in taxation or by restructuring debt.
The goal of ending Aids by 2030 is still achievable, Stegling believes. “I think we have a very short window of opportunity now, in the next two, three months, to continue telling people that we can do it.
“I keep on reminding people, ‘look, we need to get back to that same energy that we had when people were telling us treatment can’t be available in the global south, right?’ And we didn’t accept it. We made it happen.
“We have national governments now who are also very adamant, because they can see what can happen, and they want to make it happen for their own populations.”
