Industry-wide medical trend pressures contributed to Highmark’s 2024 losses.
KEY TAKEAWAYS
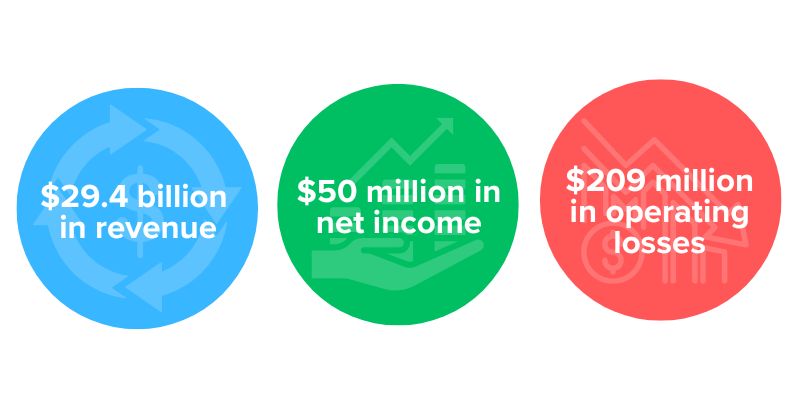
Highmark Health Plans saw negative operating performance due to industry wide medical trend costs.
Allegheny Health Network reports 9% total revenue growth and improved operating performance year-over-year.
Highmark Health Plans reported a negative operating performance, citing “industry wide medical trend pressures that continued into the fourth quarter of 2024” as the main contributor.
Despite this loss, two sectors within Highmark Health saw improved operating performance. Both United Concordia Dental and HM Insurance Group’s operating performances remained steady, fueled by increased dental membership and pricing discipline.
Allegheny Health Network (AHN), Highmark Health's provider network, also saw operating improvements that were driven by increased patient volumes across all care delivery areas.
Highmark Health’s balance sheet remained strong with $11.7 billion in cash and investments and net assets of $9.8 billion as of December 31, 2024.
The breakdown
Living Health model
A big part of Highmark’s health Plan membership increase came from efforts in its Living Health model, which allowed all eligible health plan members to gain access to the My Highmark app. The app connects patients to care in a variety of ways such as simplified bill payment and real time personalized recommendation through artificial intelligence.
“We also continue to expand our living health suite of digital and virtual health solutions. At the start of 2024, we launched mental well-being powered by spring health, increasing member access to mental health care by over 40%,” said Highmark Health president and CEO of Daivd Holmberg on an earnings call.
Highmark Health Plans
Operating revenue brought in from Highmark Health Plans was $22 billion, along with $166 million on operating losses through the year-end of 2024. The losses in this business sector were brought on by “increasing headwinds from rising health care usage, continued effects of Medicaid redeterminations, and high prescription drug costs, particularly GLP-1s,” according to the report.
“We're working through proper research strategies to address these challenges and improve performance. For instance, rapidly approaching a high cost of prescription drugs,” said Highmark Health CFO Carl Daley.
In 2024, Highmark also added a Medicaid segment in West Virginia, as well as entering the Southeastern Pennsylvania market, where it gained more than 70,000 new members. The organization also reported increased core health plan and Blue Card membership for Jan. 2025 compared to the same period last year, reporting 7.1 million members. Highmark Health Plans remain the largest health insurer in Pennsylvania, Delaware, West Virginia, and western New York.
Allegheny Health Network
AHN saw its total revenue increase by 9% year-over-year to $5.1 billion, and its operating loss also improved by 15% to $147 million compared to the same period last year. This was in part driven by increased patient volumes. In total, the provider network saw $115 million in earnings before EBITDA for the year-end of 2024.
Through Dec. 31, 2024, AHN saw patient volume increases in the following compared to the same period in 2023:
- 3% increase in inpatient discharges and observations
- 6% increase in outpatient registrations
- 5% increase in physician visits
- 5% increase in emergency room visits
Community and workforce
During the call, Holmberg addressed Highmark’s commitment to its communities, in which it has funded partnerships with community programs through its Highmark Bright Blue Futures program and donated roughly $53 million.
Holmberg stressed that as a nonprofit organization, commitment to its communities is top of mind. “No matter what happens in our industry, we will continue to invest in transforming health and creating high value jobs for the communities we serve,” Holmberg said.
Holmberg also addressed the layoffs made in January to its information technology subsidiary enGen, in which 207 employees were fired, including 86 in Western Pennsylvania and 41 in the central part of the state. EnGen jobs were also cut in eastern Pennsylvania, West Virginia, western New York, and other states.
“We will not cut costs anywhere that undermines our commitment to providing high quality care and creating remarkable health experiences,” Holmberg said. “Our approach does mean sometimes we eliminate jobs, but it also allows us to identify opportunities to shift people into new roles and create new high value jobs. We hired 6000 people in 2024. That's also part of our performance story.”
Marie DeFreitas is the CFO editor for HealthLeaders.
