SnapshotNIR Used to Predict Skin Flap Necrosis Intra-Operatively in Oncologic Resection Reconstruction
Tissue oxygen saturation measurement accurately predicted skin flap necrosis in oncologic breast reconstruction surgeries.
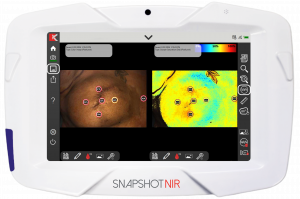
CALGARY, ALBERTA, CANADA, June 11, 2024 /EINPresswire.com/ -- A new study was published demonstrating the successful use of near-infrared spectroscopy (NIRS) imaging with SnapshotNIR to predict potential skin flap necrosis (SFN) following post-mastectomy breast reconstruction (PMBR). The study compared the standard clinical evaluation protocol to SnapshotNIR images of tissue oxygen saturation (StO2) to predict necrosis (1). In this assessor-blinded study of 102 patients, comparative Snapshot images were taken intra-operatively after wound closure and at four weeks during follow-up.
“The study found that StO2 measurements ≤60% were predictive of SFN and supported clinical consideration to perform debridement or other interventions.”
Breast cancer makes up 30% of all newly diagnosed cancers in the US, and breast reconstruction techniques are being offered by surgeons and delivered at higher rates, making the adoption of valuable and effective MedTech an essential tool in patient outcomes (2). An unfortunate side effect of oncologic reconstruction surgeries can include the requirement of further operations in many patients’ cases due to complications like skin flap necrosis, infection, or dehiscence (3, 4), and investigations such as this study can help drive innovative surgical solutions.
Rates of SFN vary across individual studies and different types of reconstruction from 5-30% (3-5), therefore, being able to reduce even a fraction of these occurrences can vastly improve surgical outcomes. Providing evidence to reduce the consequences of this life-saving surgery can enhance the patient’s post-operative quality of life and satisfaction.
“The results of this study indicate that NIRS can be used intra- and post-operatively to augment the clinical examination to guide clinical decision-making.”
SnapshotNIR measures StO2, oxyhemoglobin and deoxyhemoglobin using reflectance-based technology, in a non-invasive, non-contact handheld device. Its use can be effective in the surgical industry intra- and post-operatively in patient monitoring of interventions as seen in this open-access study. Snapshot has a unique, proprietary algorithm that can be used by clinicians on all skin types with varying levels of melanin content, specifically in the surgical sector including PMBR and oncologic resection reconstruction. Evidence supporting the use of SnapshotNIR to predict necrotic skin flaps can be directly translated into the field and assist surgeons’ decisions to provide appropriate interventions.
As MedTech evolves, research is required to support the use of it and Kent Imaging is excited to see more work from the research team behind this ground-breaking paper: Hill at the Section of Plastic Surgery, University of Calgary, Cumming School of Medicine, Calgary, AB, Canada; Kinaschuk at the Department of Family Medicine, University of Calgary, Cumming School of Medicine, Calgary, AB, Canada; and Temple-Oberle at the Department of Surgery and Oncology, Foothills Medical Centre, Calgary, AB, Canada.
About Kent Imaging
Kent Imaging, located in Calgary, Alberta, Canada, is a leading innovator in near-infrared tissue oxygenation imaging, which develops, manufactures, and markets medical technology that supports real-time decision-making in wound care, vascular and surgical subspecialties. Kent holds multiple patents in oxygen imaging technology and continues to provide innovative and advanced diagnostic imaging solutions to aid healthcare systems nationally and internationally. SnapshotNIR is supported by clinical evidence demonstrating its ability to help improve clinical decision-making in wound care and reduce healing time. Since receiving FDA and Health Canada clearance in 2017, the technology has been featured in several published articles and peer-reviewed posters. Applying the knowledge gained from clinical trials to patient care promotes consistency of treatment and optimal outcomes.
References:
1. Hill, W.F. MD; Kinaschuk, K. MD; Temple-Oberle, C. MD, MSc, FRCSC*. Intraoperative Near-infrared Spectroscopy Can Predict Skin Flap Necrosis. Plastic & Reconstructive Surgery-Global Open 12(3):p e5669, March 2024. | DOI: 10.1097/GOX.0000000000005669.
2. Breast Cancer Facts and Statistics. Mar 12, 2024, retrieved on April 4, 2024. Available at: https://www.breastcancer.org/facts-statistics.
3. Phillips BT, Lanier ST, Conkling N, Wang ED, Dagum AB, Ganz JC, Khan SU, Bui DT. Intraoperative perfusion techniques can accurately predict mastectomy skin flap necrosis in breast reconstruction: results of a prospective trial. Plastic and reconstructive surgery. 2012 May 1;129(5):778e-88e.
4. Antony AK, Mehrara BM, McCarthy CM, Zhong T, Kropf N, Disa JJ, Pusic A, Cordeiro PG. Salvage of tissue expander in the setting of mastectomy flap necrosis: a 13-year experience using timed excision with continued expansion. Plastic and reconstructive surgery. 2009 Aug 1;124(2):356-63.
5. Potter S, Conroy EJ, Cutress RI, Williamson PR, Whisker L, Thrush S, Skillman J, Barnes NL, Mylvaganam S, Teasdale E, Jain A. Short-term safety outcomes of mastectomy and immediate implant-based breast reconstruction with and without mesh (iBRA): a multicentre, prospective cohort study. The Lancet Oncology. 2019 Feb 1;20(2):254-66.
Leah Pavlick
Kent Imaging Inc.
leah@kentimaging.com
Distribution channels: Business & Economy, Companies, Healthcare & Pharmaceuticals Industry, Science, Technology
Legal Disclaimer:
EIN Presswire provides this news content "as is" without warranty of any kind. We do not accept any responsibility or liability for the accuracy, content, images, videos, licenses, completeness, legality, or reliability of the information contained in this article. If you have any complaints or copyright issues related to this article, kindly contact the author above.
Submit your press release